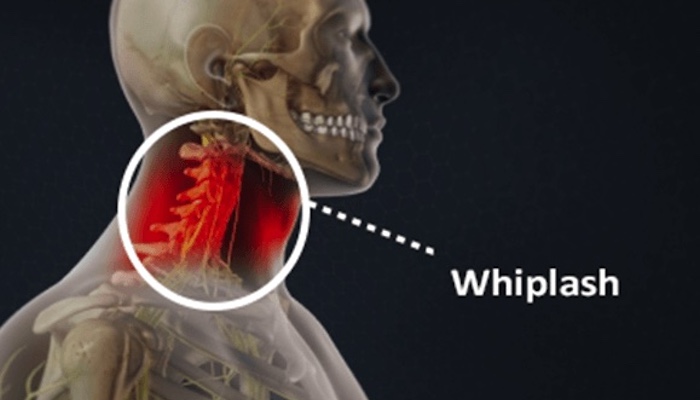
Whiplash is diagnosed by a clinician when the patient reports some neck pain in the aftermath of trauma capable of causing an acceleration-deceleration injury – most commonly a motor vehicle accident.
However, the specifics of a whiplash diagnosis can be complex and have long been the subject of controversy. In the mid-and late-1800s, there were increasingly common disputes regarding train passengers injured in collisions and whether their claims of the mysterious “railway spine” were legitimate. In modern society, the debates are sometimes similar with people claiming chronic pain and psychological distress from a motor vehicle crash without having independently verifiable signs of physical injury from the accident.
While today’s medical community better understands and accepts the oftentimes perplexing, multi-faceted nature of whiplash-associated disorders, proving the exact medical reason for all ongoing symptoms whether physical or psychological can still be elusive.
Patient History Collected for Whiplash
When a patient visits the doctor for neck pain symptoms potentially related to a whiplash injury, the following steps will likely occur:
- Complete patient history
- Physical examination
- Diagnostic imaging (only if a fracture or neurological problem is suspected)
For the complete patient history, a full medical background will be gathered first, including family history, any pre-existing conditions, and other health considerations, such as medications or previous injuries, etc. Then questions will be asked regarding the current symptoms and how they started:
- How was the neck injured? Was it a car crash or some other incident?
- When did the pain and/or symptoms start? Were the symptoms present immediately after the accident, or did they take a few hours or days to appear?
- What is the nature of the pain? Where does it hurt, and how much does it hurt? Does the pain come and go, or is it constant? Does the pain radiate down the shoulders and arms?
Depending on the answers given, the doctor’s line of questioning can go in various directions to get relevant information regarding a patient’s specific symptoms and situation.
Physical Exam for Whiplash
Once a complete history is taken, the doctor will perform a physical exam in the office. This usually starts with:
- Observation. The patient’s posture and neck will be examined for any misalignment or other abnormalities.
- Palpation. The doctor will feel different sections of the neck to check for tenderness or tightness.
- Range of motion. The doctor will test the patient’s neck mobility in rotation and movements from side to side, as well as up and down.
If anything in the patient’s reported symptoms or initial physical exam suggests the possibility of an irritated nerve such as pain, tingling, or weakness radiating into the shoulder, arm, or hand the doctor might further investigate with these in-office tests:
- Reflexes. A rubber hammer can be used to test whether nerves in the neck are sending the correct signals to the biceps, triceps, and forearm.
- Muscle power. Basic tests to see if the shoulders, arms, or hands exhibit any significant weakness.
- Sensation. Depending on where abnormal sensations are experienced, such as tingling in the thumb instead of the pinky, can help narrow down which cervical spinal segment is likelier to be the source of the problem.
Once the physical exam is complete, the doctor will usually have enough information to start devising a treatment plan or to at least know which diagnostic test(s) might be helpful to try next.
Diagnostic Imaging
If a fracture or neurological problem is suspected, the doctor will probably order diagnostic imaging to learn more. Some options could include:
- X-ray. Also called a radiograph, this imaging shows the bones and can help identify the location of a fracture.
- MRI scan. A magnetic resonance imaging (MRI) scan shows bones and soft tissues. While an MRI’s view of bones is not as good as an X-ray, the MRI is better for showing potential damage to soft tissues, such as muscles, ligaments, intervertebral discs, or even the brain.
- CT scan. A computed tomography (CT) scan uses X-rays and combines them into better images with a computer. In the past, a myelogram – a test that enables better viewing of the spinal canal, discs, and neural foramina by injecting dye through a spinal tap — was often used in conjunction with a CT scan. However, although it is still a useful test in certain situations, the CT scan with myelogram is not as commonly used today when checking on neck pain, in part because of the MRI’s increased popularity and some risks associated with myelogram (possibility of infection from spinal tap) and CT scan (radiation dose that is not present in MRI).
- Bone scan. Usually not the first imaging choice due to a significantly higher radiation dose, but a bone scan can be useful in detecting tiny fractures.
It is important to note that not all types or locations of injuries in the neck can be seen via imaging. Furthermore, an injury or misalignment detected via imaging is not necessarily the source of pain.
Quebec Task Force WAD Classification
In 1995, the Quebec Task Force came together to research the medical literature of whiplash-associated disorders and help bring clarity to how they are diagnosed and treated. The task force’s resulting classification system became widely adopted, but there is disagreement within the medical community as to its effectiveness.
The Quebec Task Force’s classification system for whiplash-associated disorders separated them into five different grades as follows:
Grade 0 - The patient does not complain about neck pain and has no physical signs.
Grade I - Patient complains of neck pain, stiffness, or tenderness, but has no physical signs, i.e., no limitation in range of motion, no loss of strength, no swelling, etc.
Grade II - The patient might have the same neck complaints as Grade I, but the clinician also finds physical signs, such as decreased range of motion and point tenderness.
Grade III - The patient might have the same neck complaints and physical signs as Grade II, but a clinician also finds neurological signs, such as weaker muscles or sensory problems.
Grade IV - The patient has neck complaints and a fracture or dislocation is found.
With the Quebec Task Force’s classification system, the vast majority of patients with whiplash-associated disorders are classified as Grade II. Some people argue that Grade II needs more subgroups to further distinguish between these patients and thus offer them treatment programs for their specific needs. A related criticism of the Quebec Task Force’s classification system is that it does not take into account the complex psychological factors that could be present in a patient, which can also greatly affect the type of treatment needed.
Precision Pain Care and Rehabilitation has two convenient locations in Richmond Hill – Queens, and New Hyde Park – Long Island. Call the Queens office at (718) 215-1888 or (516) 419-4480 for the Long Island office to arrange an appointment with our Interventional Pain Management Specialists, Dr. Jeffrey Chacko or Dr. Sonny Ahluwalia.













