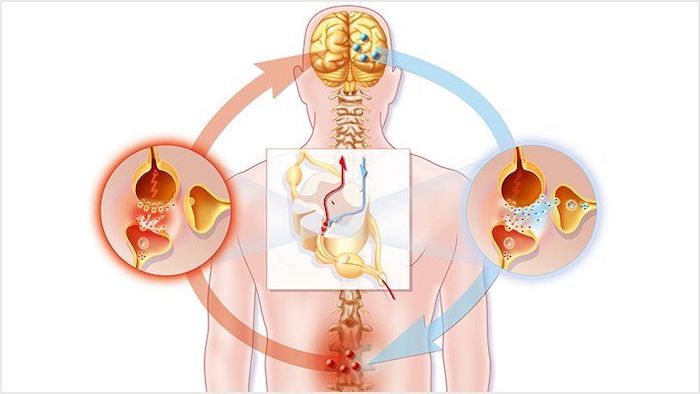
When you feel pain, it is due to certain chemical and electric signals that are exchanged between the site of injury and the brain. These signals are carried through your nerves. Neuropathic pain occurs when there is an injury or damage to a single nerve or group of nerves.
Neuropathic pain differs from the more commonly understood nociceptive pain.
- Neuropathic pain occurs due to inflammation, irritation, or compression of the neural tissue.
- Nociceptive pain is the body’s response to painful stimuli, such as a pulled back muscle or broken bone, and does not relate to an injury of the nerve itself.
Here are a few pointers to help you identify neuropathic pain and its common treatment methods.
How Neuropathic Pain May Occur in The Lower Back
Neuropathic pain may originate through one or more of the following mechanisms:
- Local neuropathic pain. When nerve tissue grows into a degenerated intervertebral disc, localized nerve pain or discogenic pain may occur.
- Mechanical neuropathic pain. When a nerve root is compressed as it exits the spine (such as from a herniated disc or narrow bony opening for the nerve), nerve pain may occur along with the distribution of the nerve.
- Inflammatory neuropathic pain. When the nerve roots are irritated due to chemical substances that leak out of herniated or degenerated discs, the resulting inflammation and damage may cause pain to occur along with the distribution of the nerve.
Mechanical and inflammatory neuropathic pain typically travels down the leg and is called radicular pain (pain arising from nerve roots). This pain is commonly referred to as sciatica.
Common Symptoms of Neuropathic Lower Back Pain
Neuropathic pain symptoms may be variable and unpredictable. It is also common for neuropathic and nociceptive pain to occur together in the lower back.
A few common features of neuropathic pain include:
- Sharp, stabbing, shooting, and/or shock-like pain that radiates from the lower back into your leg
- Burning sensation in your lower back and/or legs
- Pricking (pins and needles) sensation in your back and/or legs
- Tingling, weakness, and/or numbness, typically felt in your legs
Acute, localized pain or a dull ache may occur in your lower back in case of discogenic pain.
Causes and Other Characteristics of Neuropathic Lower Back Pain
Neuropathic pain may be caused by nerve damage due to inflammation, metabolic conditions (diabetes), infections (herpes zoster), trauma, toxins, and tumors.
While neuropathic pain can go away on its own, it often becomes chronic. It is frequently the result of an injury or trauma that compresses or impinges on a nerve, damaging it beyond repair. For example, a herniated disc may push against a nerve root(s), which can send neuropathic pain signals to the brain. Over time, the herniated disc may stop compressing the nerve, but the nerve tissue can become damaged and continue to send faulty pain signals to the brain.
Managing Neuropathic Pain
In treating neuropathic pain, a combination of medical treatments and lifestyle modifications, such as staying active is recommended.
Treatment usually includes some combination of:
- Self-care heat and ice therapy, using correct posture, and activity modification
- Physical therapy and exercise
- Cognitive-behavioral therapy
- Transcutaneous electrical nerve stimulation (TENS)
- Invasive procedures, such as epidural steroid injections (ESIs) and spinal cord stimulation (SCS)
Medications are usually less effective in controlling neuropathic pain and may be more ineffective if your pain is chronic. Typically, prescription medications, such as tricyclic antidepressants, anticonvulsants, opioids, and tramadol are used. Acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs) are usually used to treat the associated nociceptive pain but have less or no effect on neuropathic pain.
Neuropathic pain can be difficult to identify and sometimes challenging to manage. Talk with your doctor to get a correct diagnosis of your pain condition. A doctor can conduct specific tests, rule out serious underlying conditions, such as tumors, and formulate an effective treatment plan for your neuropathic pain.
Precision Pain Care and Rehabilitation has two convenient locations in Richmond Hill – Queens and New Hyde Park – Long Island. Call the Richmond Hill office at (718) 215-1888, or (516) 419-4480 for the Long Island office, to arrange an appointment with our Interventional Pain Management Specialist, Dr. Jeffrey Chacko.













