People showing symptoms of a lumbar herniated disc can expect the doctor to conduct a detailed interview and perform a thorough physical exam.
Questions to Expect
Questions about when and how the pain started are typical, particularly if there was any type of traumatic injury. Other questions may focus on:
- The type of pain. The patient may be asked to describe the pain, including its location and which activities or positions make it better or worse.
- Medical conditions. Other medical conditions could be a factor. Osteoporosis, for instance, increases the risk of a fracture.
- Home and work life. Having a physically demanding job or regularly performing repairs or other strenuous work at home can put pressure on a lumbar disc.
- Medical history. The doctor will probably inquire about previous treatments or injuries.
- Family medical history. A lumbar herniated disc is more likely if a family member has the condition.
Any experience with depression or anxiety should also be part of the discussion, since this information may be helpful in planning treatment.
Physical Exam to Diagnose Lumbar Herniated Disc
The physical examination is crucial to the diagnosis, and usually includes observation of the patient bending and stretching. These assessments are typical:
- Neurological check. To determine whether there is a neurological problem, the doctor typically looks for signs of loss of sensation, such as numbness, and weakness in the leg and foot. The patient may be asked to walk normally and on tiptoes to check for a condition called foot drop, in which the muscles used to flex the ankles and toes are weakened. Muscle strength and reflexes in other areas are also likely to be checked. Reflexes may be slower than normal or nonexistent.
- Range of motion tests. The patient may be asked to lean forward and back and bend from side to side.
- Leg raise test. One common stretch to test for a herniated disc is the straight leg raise, or LaSegue, test. For this test, the patient lies down flat on the back and the doctor gently raises the affected leg until the pain is felt. If pain occurs when the leg is raised at a 30 to 70-degree angle, it is considered a sign of lumbar disc herniation. If raising the unaffected leg hurts the affected leg, it also indicates that a nerve root is impinged or irritated. Variations on these stretches include performing the tests from a seated position or while the legs are crossed. Some of the medical literature has found the straight-leg-raise test is not as helpful for indicating lumbar herniated discs in people older than age 60.12
- Vital signs check. An increase in pulse rate or blood pressure can be an indication of pain, and elevated temperature may be a sign of infection.
- Gait monitoring. The doctor will observe whether the patient appears to be walking slowly due to pain, or with an abnormal gait.
- Lumbar spine area exam. If there is inflammation in the lumbar spine, the skin may appear abnormal or sensitive to touch.
If the doctor sees no signs of a serious problem, the pain is not severe, and there has been no traumatic injury, imaging tests may not be necessary at this point. Some doctors prefer to have the patient wait to see whether the symptoms go away within six weeks, as happens for most people.
Imaging Tests for Lumbar Herniated Disc
Imaging tests may be included at the initial visit to rule out other possible causes of the patient's symptoms such as a fracture, tumor, infection, or caudal equina syndrome.
These are the typical imaging tests used to detect a herniated disc:
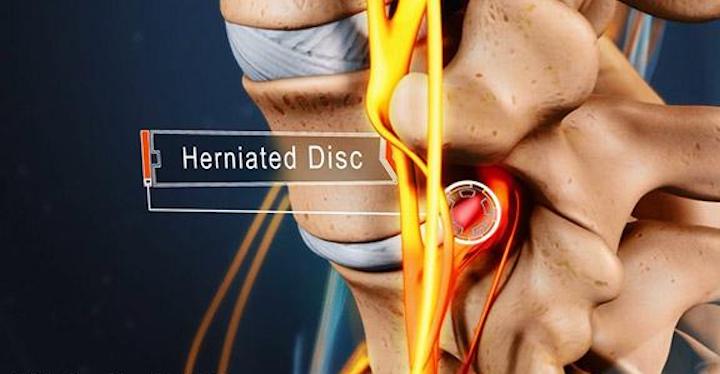
- MRI (magnetic resonance imaging) usually provides the most accurate assessment of the lumbar spine area, showing where a herniation has occurred and which nerves are affected. Often, an MRI scan is ordered to aid surgical planning. It can show where the herniated disc is and how it is impinging on the nerve root.
- CT (computed tomography) scan is more likely if there is a reason an MRI is not advised.
- X-rays are mainly used to rule out problems such as a broken bone, bone abnormalities, infection, tumor, or problems with the alignment of the spine. X-rays are not typically used on their own to diagnose a herniated disc.
- CT myelogram is a computed tomography scan using contrast dye in the spinal fluid, with X-rays to view the dye. This can show both the size and location of a herniation but is invasive.
- Electromyography (EMG) can pinpoint which nerve root is impacted.
Imaging tests alone cannot diagnose a herniated disc. In some cases, an MRI scan may show an advanced lumbar herniated disc, but the person has no pain or other symptoms.13
The reason for the lack of symptoms is not clear, but some medical professionals speculate that disc herniation is even more widespread than commonly thought and often a natural part of aging.
A major challenge in diagnosing a lumbar herniated disc is the need to distinguish the condition from other causes. These other causes must be ruled out to reach the correct diagnosis and begin treatment.
If you are suffering from pain, please contact our office at (516) 419-4480 or (718) 215-1888 to arrange an appointment with our Interventional Pain Management Specialist, Dr. Jeffrey Chacko.













