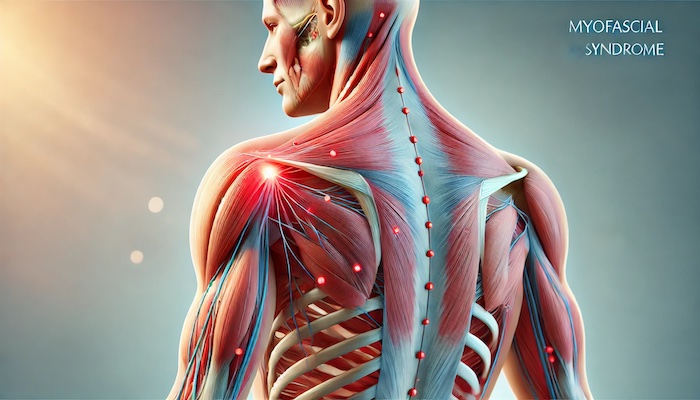
Myofascial Pain Syndrome (MPS) is a chronic pain disorder caused by inflammation in the fascia—the connective tissue covering muscles. Unlike common muscle soreness, MPS is characterized by painful trigger points, and small knots in the muscle that can lead to referred pain, making the pain spread to other areas of the body. This complex syndrome can lead to significant discomfort and impact daily function, requiring a specialized approach to diagnosis and treatment.
What is Myofascial Pain Syndrome?
MPS is commonly seen in people who experience repetitive muscle strain, poor posture, or injury. It is often mistaken for other pain conditions, as the symptoms can be quite similar to those of fibromyalgia and other musculoskeletal disorders. However, MPS has unique markers, such as palpable knots or trigger points within the muscles, which can be intensely painful and may radiate pain to unrelated areas. Patients frequently describe a deep, aching sensation, stiffness, and limited range of motion in affected muscles.
Symptoms of Myofascial Pain Syndrome
The primary symptom of MPS is muscle pain with the presence of trigger points. Other symptoms include:
- Pain that worsens with stress or activity
- Persistent pain that doesn’t improve with rest
- Referred pain in unrelated areas
- Difficulty sleeping due to muscle pain
- Limited movement and stiffness
Causes and Risk Factors
MPS often stems from a specific muscle strain or repetitive muscle use. Physical or emotional stress, as well as poor posture, can also exacerbate or trigger myofascial pain. Conditions like arthritis or other musculoskeletal disorders may increase the likelihood of developing MPS. Factors such as a sedentary lifestyle, anxiety, and depression may worsen the severity of symptoms, making it crucial to address lifestyle and mental health alongside physical symptoms.
The Role of Interventional Pain Management
Interventional pain management offers a multidisciplinary approach to managing MPS effectively. By targeting the pain at its source, these techniques help alleviate symptoms and improve quality of life. Unlike traditional pain management, interventional pain management uses advanced procedures to target pain directly rather than relying solely on medication. This approach can include trigger point injections, nerve blocks, and minimally invasive procedures tailored to the needs of each patient.
Effective Interventional Techniques for MPS
Here are some common interventional techniques used to manage myofascial pain:
- Trigger Point Injections: A specialized injection of anesthetic and anti-inflammatory medications directly into the trigger point can help reduce pain and relax the muscle, providing immediate relief. This method is often used for patients with stubborn pain that doesn’t respond to other treatments.
- Ultrasound-Guided Therapy: Using ultrasound imaging, physicians can pinpoint specific areas of inflammation and pain. This non-invasive method helps guide treatments, such as injections or electrical stimulation, with precision, ensuring relief in the exact spot where it’s needed.
- Dry Needling: Dry needling is another technique used to deactivate trigger points. By inserting thin needles into the skin and muscle, physicians stimulate the muscle tissue, which reduces tension and alleviates it. Although dry needling and acupuncture may appear similar, dry needling specifically targets muscle pain linked to trigger points.
- Nerve Blocks: This technique involves an injection to block pain signals along specific nerves. Although more commonly used in cases of neuropathic pain, nerve blocks can help patients with MPS by providing temporary pain relief and reducing muscle tension.
Lifestyle and Rehabilitation
A comprehensive MPS treatment plan often includes physical therapy, stretching, and strengthening exercises to restore normal muscle function. Incorporating stress management, adequate sleep, and hydration also play a critical role in managing symptoms long-term. Therapies like yoga, massage, and chiropractic care may complement interventional techniques, enhancing their effectiveness.
Benefits of Interventional Pain Management for MPS
Interventional pain management has shown substantial promise in alleviating chronic pain and enhancing patients' quality of life. By addressing pain at its root, patients often report:
- Improved mobility and flexibility
- Decreased reliance on pain medications
- Enhanced quality of sleep and overall well-being
- Long-term relief from muscle pain and stiffness
Data on MPS and Pain Management Success
Studies show that a targeted approach to MPS using interventional techniques significantly improves patient outcomes. For example, patients undergoing trigger point injections report around a 50-80% reduction in pain, while those combining physical therapy with dry needling experience notable improvements in mobility and pain relief. Tailoring interventional treatments based on individual needs has led to higher patient satisfaction and a reduced need for repeated procedures.
Moving Forward with Precision Care
If you or a loved one struggles with persistent muscle pain, seeking care from specialists in interventional pain management can be a game-changer. With a thorough understanding of myofascial pain, these specialists offer tailored solutions that address the unique challenges MPS presents. By combining medical expertise with innovative techniques, Precision Pain Care and Rehabilitation is committed to helping patients regain their mobility, function, and quality of life.
Early intervention, coupled with personalized care, can make a significant difference in managing MPS. With the right treatment plan, it’s possible to break free from chronic muscle pain and restore function to the fullest.
Precision Pain Care and Rehabilitation has two convenient locations in Richmond Hill – Queens, and New Hyde Park – Long Island. Call the Queens office at (718) 215-1888 or (516) 419-4480 for the Long Island office to arrange an appointment with our Interventional Pain Management Specialists, Dr. Jeffrey Chacko or Dr. Sonny Ahluwalia.













