Fibromyalgia is often thought of as a new diagnosis! Stigma often results in people thinking that fibromyalgia is just a name that has been thrown on a group of symptoms that doctors can give when they can’t figure out what else is wrong. These misconceptions are damaging and far from true.
Fibromyalgia is a valid diagnosis in its own right, and is far from a new disorder; it has a long history, as explained here, “Its definition and content have changed repeatedly in the 110 years of its existence.”
Rheumatism In 1592
Back to 1592 mentions of muscular pain and stiffness can be found in literature and scientific studies. Back then, medical professionals didn’t have all of the equipment and technology that we do now, so often there weren’t as many specific and individual names for diagnoses. In 1592, a French doctor called Guillaume de Baillou, came up with the name ‘Rheumatism’, which was a term then used to describe muscular pain that didn’t come from an injury. This would have covered chronic conditions including many forms of arthritis and fibromyalgia.
The next development came when doctors started to use the term ‘muscular rheumatism’ about conditions that didn’t cause what they defined as deformity or a change in the structure of the body. For example, osteoarthritis wears down the cartilage around the bone, so it changes the shape of the joint, whereas, with fibromyalgia, there aren’t physical changes caused to the body.
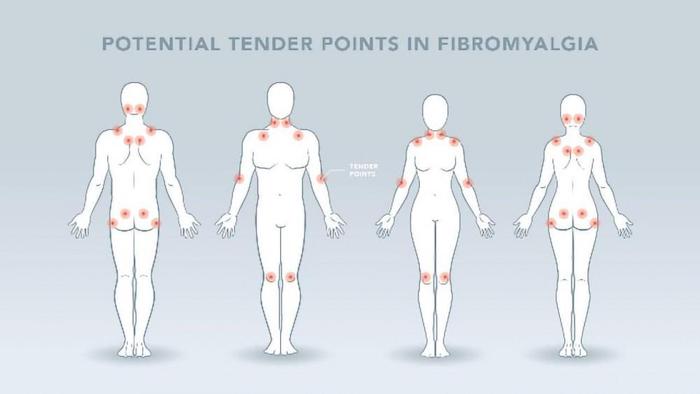
Discovering The Tender Points
A Scottish surgeon named William Balfour was the first to start developing theories to help doctors understand this sort of pain; in 1815 he realized that there were tender points around the body which were more reactive to pain and which indicated this type of muscular rheumatism. These tender points were used more recently to diagnose fibromyalgia, although now this is not a definitive indication of the disorder. William started to understand that inflammation played a key part in this type of pain. This study explains that “Balfour (1816) noted indurated nodules, tender on pressure, with pains radiating out to surrounding areas, the treatment being by ‘friction, percussion, and compression’ to these nodules.”
Later down the line in 1880, a doctor from France called Francios Valleix started to theorize that pain was traveling from these tender points and that it was affecting other areas of the body; he named this ‘neuralgia’. Around that time scientists were doing a lot more research into this type of pain; they considered theories such as the problem coming from the actual muscle itself as well as the nervous system being overactive; this could align with what we now know today is central sensitization.
Sir William Gowers and Fibrositis
As we moved into the 1900s, the symptoms of fibromyalgia were given other names. In 1904, the name ‘fibrositis’ was presented by Sir William Gowers from Britain, and this would be the name that remained in use for many years to follow as explained here. The symptoms of fibrositis match those of fibromyalgia very accurately; they are described as pain, sensitivity to pressure, fatigue, problems with sleep, temperature sensitivity, and flaring in symptoms after activity.
In 1913, rest was thought to be helpful for chronic pain, which is understandable as when the body is in pain it’s usually injured. Now we understand that exercise is important in treating pain, but then this understanding was not developed. This study from 1913 explains that “confinement to bed may be necessary, and it is important to recognize the beneficial influence of rest in such cases.” In later stages of the treatment, light exercise was recommended, “The exercises should be performed on rising in the morning, and should not occupy more than from ten to fifteen minutes.”
Treatment often included electrodes to the painful areas, which thankfully is not used now, in a process called ionization. The heat was put onto the skin, then electric currents were used on top of the heat, which they believed reduced pain as explained here, “The strength of the current that should be employed varies with individual patients, but should range from 15 to 40 milliamperes. The ionization lasts for twenty minutes, and should be repeated daily if the skin will stand the treatment’ otherwise it should be used on alternate days.” Other treatments in that era can still be incorporated today including massage, relaxation, and a healthy diet.
The type of underwear that patients wore was thought to influence fibrositis, as well as where you lived! Medical professionals believed that living above good drainage and at a good elevation was important, which when you think about it could perhaps have reduced dampness which would aggravate symptoms. However, it was believed that where you lived could be the cause of fibrositis as stated here, “Many of the gravel sites lauded by house agents are veritable traps for the development of fibrositis.”
Discovering Psychological Factors
As our knowledge of the nervous system started to develop in the early 1900s, we gained a deeper understanding of how our bodies produce and experience pain. During World War II, doctors began to realize that there was a significant emotional and stress-related connection to pain. Soldiers who did not have injuries, inflammation, or any sort of degeneration in their joints and muscles, were experiencing fibrositis.
Doctors started to realize that these soldiers were going through a great deal of stress, fear, and emotional turmoil; they understood that these emotional responses were causing and worsening the soldier’s pain. This started the ongoing confusion and debate in the scientific community about what was causing the symptoms, whether it was physical or psychological.
When 1949 came around, a leading rheumatology textbook emphasized the symptoms of fibrositis and talked about the theories around its cause. Along with a previous infection or physical injury, a significant step was that it also mentioned trauma and psychological factors.
Looking back, we can see that the term fibrositis may have included several chronic pain diagnoses which now have individual names. An even more accurate set of symptoms that match what we know as fibromyalgia today came in 1968 from a researcher named Eugene F. Traut. He talked about widespread pain, including pain, being present in various areas of the body about the spinal axes, which you can see in the present-day definition of fibromyalgia. He talked about aching, stiffness, fatigue, stomach problems, headaches, poor sleep, mental health issues such as anxiety (although then it was described as ‘being worry worts’), tender points, and emotional influence.
Interesting when talking about treatment, Eugene states in his study, “The immediate treatment usually includes the administration of analgesics, immobilization of the affected area, and infiltration of the trigger points with procaine and adrenocortical steroids.” So, while now we understand that exercise and not avoiding movement is a pivotal aspect of treating chronic pain, back then they still treated this pain with rest as they did with acute pain.
The next significant development came not long after that from Hugh A. Smythe, who built on the existing research and wrote a book on fibrositis. He investigated the emotional aspect of this disorder is far more detail along with non-restorative sleep and the tender points.
The Name Fibromyalgia
In 1976, P.K. Hench developed the name Fibromyalgia as stated here: ‘fibro’ means connective tissues, ‘my’ means muscle, and ‘algia’ means pain. Doctors still didn’t understand fibromyalgia and often the term fibrositis was still used, but over the coming years, more research would lead to a deeper understanding.
In 1981, Muhammed Yunus led a study that found additional symptoms of fibromyalgia, including irritable bowel syndrome (IBS), swelling, and paresthesia, meaning abnormal sensations such as pins and needles. From his paper, a new criterion for diagnosing fibromyalgia was developed, enabling medical professionals to differentiate it from other chronic pain diagnoses more accurately.
In 1986 studies to treat the symptoms of fibromyalgia using antidepressants were carried out, with some showing positive outcomes. This study from 1986 refers to the tricyclic antidepressants, but interestingly also to reducing stress, “Modest improvement follows treatment by tricyclic agents such as low-dose cyclobenzaprine and amitriptyline, by physical measures, and by the reduction in stress.”
In 1989, Muhammed Yunus published a study that gave definitive evidence of normal muscle biopsies in fibromyalgia patients, leading to more research focusing on the nervous system.
In 1990, the criteria for diagnosing fibromyalgia would be built upon and made official by the American College of Rheumatology. From there so much more research has been done and advances have been made including in 1993 with more research into central sensitization and its significance in chronic pain.
1995 brought an understanding of the change in blood flow in the brain of fibromyalgia patients, affecting areas of the brain that create pain messages. In 1997, the National Fibromyalgia Association was formed, to reduce the stigma around fibromyalgia and provide accurate information and support for patients. Other similar charities have since been formed and do wonderful work in reducing stigma and providing accurate information.
1999 allowed us to understand that genetics could play a part in patients being more likely to develop fibromyalgia. In 2005 a huge step forward came when the American College of Rheumatology released the first official guidelines to treat fibromyalgia, to provide clear guidance to medical professionals on how to help patients. In 2010, using tender points to diagnose fibromyalgia gained less emphasis, with questionnaires, elimination of other disorders, and clinical history focused on more so to reach a diagnosis. Since then, research has continued and we are learning more about fibromyalgia all the time.
What Do We Know Now?
Today we understand that fibromyalgia is a disorder in and of itself, although a great deal of stigma is still attached to it. Looking back at the long history of these symptoms, we can understand that fibromyalgia is far from a ‘new’ or ‘fad’ disorder.
Science now understands so much more about fibromyalgia and the way the brain processes pain. While a lot more is understood, the exact causes and processes of some aspects of fibromyalgia are yet to be discovered. With that being said, there are now truly effective ways to reduce symptoms and improve the quality of life for patients.
Cognitive Behavior Therapy (CBT), Acceptance and Commitment Therapy (ACT), and other mindfulness therapies can help patients, but many people are not aware of them because medical professionals are not given the training and education they need on chronic pain. You can access these therapies by advocating for yourself with your doctor or specialist.
What About the Future?
In the future research will continue into the exact causes and mechanisms of fibromyalgia, and hopefully, we will be able to get more answers which could lead to more treatments being developed.
The medical community needs to be educated on the type of therapies that are already in existence so that when people go to their doctor and are diagnosed with fibromyalgia, they are not sent away with no hope. Everyone deserves to have access to treatment that can truly help them.
Hopefully in the future stigma will be broken down around fibromyalgia and chronic pain conditions in general, not only in the medical community but also in society so that nobody feels they cannot speak out about their disorder or is left to feel alone.
The future can be bright for those with chronic pain if research continues, education and awareness are prioritized and stigma is reduced. There is hope ahead.
Precision Pain Care and Rehabilitation has four convenient locations in Richmond Hill – Queens and New Hyde Park, Lindenhurst, and Valley Stream – Long Island. Call the Queens office at (718) 215-1888, or (516) 419-4480 for the Long Island offices, to arrange an appointment with our Interventional Pain Management Specialist, Dr. Jeffrey Chacko.