At first glance, arthritis and bursitis seem similar. They’re two of the most common joint problems. They both involve inflammation, cause joint pain, and affect your ability to use the joint.
Despite these similarities, arthritis and bursitis are more different than alike. They each have a distinct cause. Additionally, the nature of your pain and the impact on your long-term health differ.
Whether you have arthritis or bursitis, the physician offers advanced interventional treatments customized to ease your pain and support your optimal health. Here’s a rundown of the differences between arthritis and bursitis.
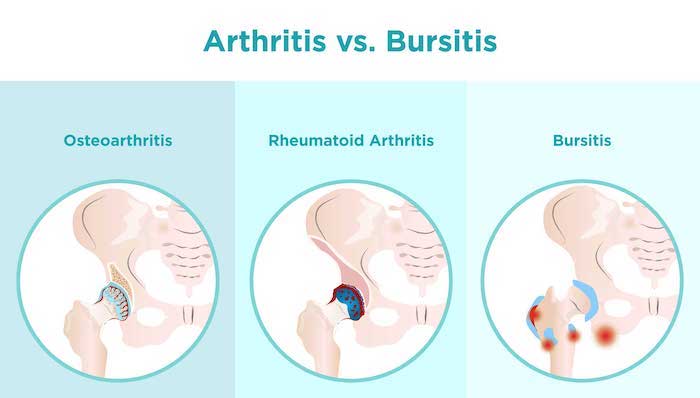
Body Structures Affected
Two of the biggest differences are found in how the diseases develop and the body structures affected by each condition:
Arthritis - The two major types of arthritis, osteoarthritis, and rheumatoid arthritis are damaged cartilage, bones, and other structures inside the joints.
Osteoarthritis begins when the cartilage breaks down. Cartilage normally protects the bones, allowing them to glide past one another as you use the joint. However, the cartilage gradually wears away because of daily stress and movement.
Over the years, more cartilage slowly wears away, inflammation develops, and the inflammation erodes the bone under the cartilage.
Rheumatoid Arthritis - Rheumatoid arthritis starts when your immune system attacks the synovial tissues lining the joint. As a result, the tissues become inflamed. The inflammation gradually erodes the bones and causes joint deformities.
Bursitis - Bursitis affects tiny, fluid-filled sacs (bursa) around the joint. Bursa is wedged between bones and soft tissues. The little sacs reduce friction between bones as they move and rub against your skin, ligaments, and tendons. When the bursa becomes inflamed, you have bursitis.
Inflammation develops because of the following:
- Repetitive use
- Prolonged pressure on the joint
- Bone spurs in the joint
- Trauma to the joint
- Infections
More than 150 bursae are in your body. Any of them can develop bursitis, but the problem most often affects your knees, shoulders, elbows, and hips.
Symptom Differences
Osteoarthritis and rheumatoid arthritis gradually damage the joint. As a result, you experience a slow but steady increase in pain and joint stiffness over the years. What begins as a slight twinge of discomfort turns into unbearable pain that stops you from using the joint.
Osteoarthritis doesn’t cause visible swelling. By comparison, rheumatoid arthritis often leads to noticeable redness and swelling around the joint.
Bursitis may develop slowly or flare up quickly. Once inflammation takes over the bursa, the condition immediately causes severe pain and limited joint movement. You may also have a noticeable swollen bump, depending on how close the bursa is to the surface.
Sometimes bursitis becomes infected. If that happens, the skin above the bursa looks red and feels warm, and you will probably have a fever.
Osteoarthritis always stays within the joint. Bursitis is always limited to the bursa. Rheumatoid arthritis is different because the inflammation can spread. As a result, you can develop inflammation and symptoms in your skin, eyes, blood vessels, lungs, and throughout the body.
Disease Duration
Arthritis is a progressive disease that causes permanent joint damage. Though each person’s osteoarthritis progresses at a different pace, the degeneration can ultimately cause such extensive joint damage that your only treatment option is a joint replacement.
Though rheumatoid arthritis also progresses and causes irreversible damage, we have medications that can keep it in remission. With early treatment, medications can slow down or prevent bone erosion caused by rheumatoid arthritis.
Bursitis is a short-term condition. It doesn’t get progressively worse or last until you need a joint replacement. Instead, bursitis responds well to rest and steroid injections that reduce inflammation.
In most cases, your bursitis improves in a few days or weeks. However, it can recur if you keep stressing the joint with the same activities.
Precision Pain Care and Rehabilitation has two convenient locations in Richmond Hill – Queens and New Hyde Park – Long Island. Call the Queens office at (718) 215-1888, or (516) 419-4480 for the Long Island office, to arrange an appointment with our Interventional Pain Management Specialist, Dr. Jeffrey Chacko.