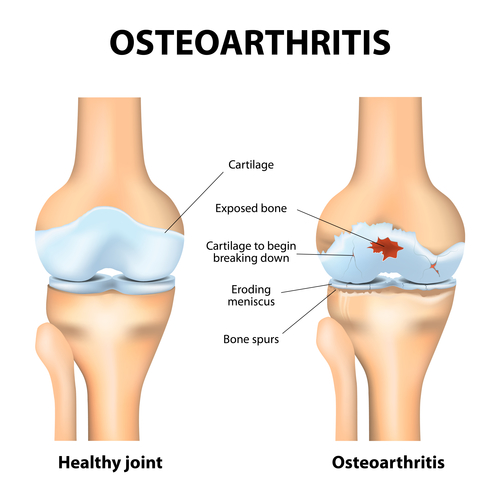
While knee osteoarthritis is often a progressive and irreversible degenerative process, functional improvement and pain control are reasonable treatment goals.
Earlier treatment intervention may improve the odds of preserving joint integrity and function for years - or even a lifetime - which can stave off debilitating pain and a possible need for joint replacement surgery.
Non-Surgical Treatments
Stem Cell & Platelet Rich Plasma (PRP): Stem Cell & Platelet Rich Plasma (PRP) procedures are the world’s most advanced regenerative injection treatments for treating knee pain due to arthritis, meniscus tears, traumatic ligament injuries, overuse conditions and other degenerative conditions.
If you have encountered an injury to the knee meniscus, cartilage, ACL or MCL ligaments, or have chronic knee pain due to a past injury or arthritis, you may be a good candidate for knee stem cell therapy or platelet rich plasma (PRP) procedures. Traditional options for patients suffering from these issues include arthroscopic knee surgery to repair ligament tears or total knee joint replacement. With both surgeries, months of rehab are required to regain strength and mobility, and the patient must be aware of and prepared for associated risks.
Physical therapy and exercise: A graduated and targeted knee strengthening and stretching exercise program is an integral component of the treatment of knee osteoarthritis. Most often, an appropriately trained physical therapist or doctor will evaluate the biomechanical issues that may contribute to the individual's knee arthritis pain. Then, they will teach the patient-specific exercises to stretch inflexible soft tissues and others that build the muscles around the knee, thereby supporting the knee joint and making it less prone to further cartilage loss.
Activity modification: While exercise is important to treating knee osteoarthritis, some types of activities and exercise will aggravate the knee joint. Certain high impact activities should be avoided, and alternatives may be identified. For example, jogging may be replaced with cycling or swimming, both of which exert less force on the knee joint. While painful knee osteoarthritis may cause someone to be less active in general, less physical activity is not advisable. In fact, inactivity is harmful and often leads to other health problems. The health care provider will work with the individual patient to find alternatives or adaptive strategies to perform daily activities that trigger pain.
Periodic rest: A little discomfort is to be expected as stiff joints loosen up in the morning or at the beginning of the exercise. However, when people feel a terrible pain that limits their ability to function normally, they should generally not try to "work through the pain." Moderate to severe knee pain is a signal that the joint needs a rest. If there is no pain relief within 2 to 4 days of rest, then the individual should seek medical attention.
Warm or cold compress: Using a warming pad or whirlpool for a few minutes can loosen a stiff knee joint making activity easier. Icing the knee joint for 15 or 20 minutes after activity can decrease swelling and provide some immediate pain relief. Heating or icing a joint is focused on improving symptoms temporarily: it does not alleviate the underlying causes of knee pain and will not improve long-term joint function by itself.
Weight loss: A diet to maintain a healthy weight can pay big dividends for those suffering from knee osteoarthritis. For every extra pound on the body, an extra three pounds of pressure is exerted on the weight-bearing knee joint. Gaining 10 pounds can mean 30 pounds more pressure on the knee with each step, as well as a significantly greater chance of developing osteoarthritis. For people who are overweight or obese, losing weight will significantly reduce pressure and strain on the knee joint, thereby alleviating symptoms and perhaps slowing the progression of knee osteoarthritis.













