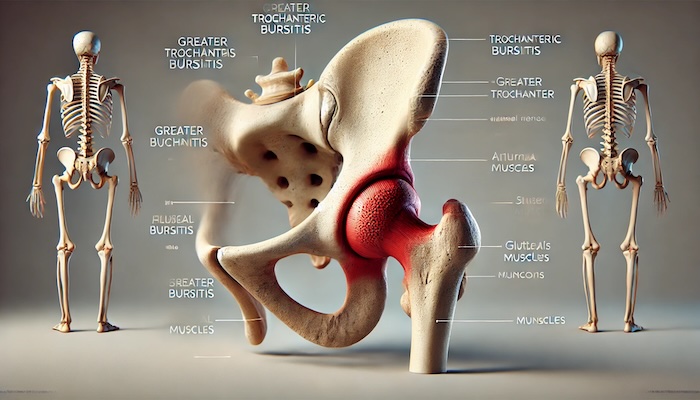
Trochanteric bursitis, also referred to as greater trochanteric pain syndrome (GTPS), is a common cause of hip pain that can significantly affect daily life. This condition involves inflammation of the trochanteric bursa, a small, fluid-filled sac located near the greater trochanter of the femur. The bursa’s primary function is to reduce friction between the bone and surrounding soft tissues during movement. When inflamed, the bursa can cause discomfort, pain, and limited mobility in the hip area.
What Causes Trochanteric Bursitis?
Trochanteric bursitis can develop due to various factors, including:
- Overuse or Repetitive Movements: High-impact activities like running, cycling, or climbing stairs can irritate the bursa and surrounding tissues.
- Injury or Trauma: A fall, direct blow to the hip, or awkward movements can lead to inflammation of the bursa.
- Poor Biomechanics: Improper posture, leg length discrepancies, or gait abnormalities can place excessive stress on the hip.
- Underlying Medical Conditions: Conditions like osteoarthritis, rheumatoid arthritis, or lumbar spine disorders can increase the risk of developing trochanteric bursitis.
- Muscle Weakness: Weakness in the gluteal muscles can lead to instability in the hip joint, increasing the likelihood of bursal irritation.
- Post-Surgical Factors: Hip surgeries, such as joint replacements, can sometimes contribute to bursitis.
Recognizing the Symptoms
The primary symptom of trochanteric bursitis is lateral hip pain, which can range from mild discomfort to severe pain. Key symptoms include:
- Pain on the Outer Side of the Hip: Tenderness near the greater trochanter is a hallmark sign.
- Pain During Activity: Pain may worsen with prolonged walking, climbing stairs, or standing for extended periods.
- Nighttime Discomfort: Lying on the affected side can exacerbate symptoms, disrupting sleep.
- Radiating Pain: Discomfort may extend down the outer thigh but typically does not affect the knee or foot.
- Stiffness and Swelling: Some individuals may experience mild swelling or stiffness in the hip region.
Diagnosis of Trochanteric Bursitis
Diagnosing trochanteric bursitis involves a thorough physical examination, medical history review, and imaging studies if needed. During the physical exam, a healthcare provider will:
- Assess tenderness over the greater trochanter.
- Evaluate range of motion and strength in the hip joint.
- Rule out other conditions, such as hip arthritis or nerve compression, using imaging tools like X-rays, ultrasounds, or MRIs.
Treatment Options for Trochanteric Bursitis
Effective management of trochanteric bursitis often requires a combination of conservative treatments, interventional therapies, and preventive strategies.
Conservative Approaches
- Rest and Activity Modification: Avoid activities that worsen the symptoms to allow the bursa to heal.
- Ice and Heat Therapy: Applying ice packs can reduce swelling, while heat can help relax tight muscles around the hip.
- Non-steroidal Anti-Inflammatory Drugs (NSAIDs): Medications like ibuprofen or naproxen can help reduce pain and inflammation.
- Stretching and Strengthening Exercises: Targeted physical therapy exercises can improve flexibility and strengthen the hip muscles, reducing stress on the bursa.
- Assistive Devices: Using a cane or crutches temporarily can relieve pressure on the hip joint.
Interventional Pain Management Techniques
At Precision Pain Care and Rehabilitation, interventional pain management strategies are tailored to the patient’s needs. These include:
- Corticosteroid Injections: These injections deliver powerful anti-inflammatory medication directly into the bursa, providing quick and effective relief.
- Platelet-Rich Plasma (PRP) Therapy: PRP therapy uses the patient’s blood to accelerate tissue healing and reduce inflammation in the affected area.
- Extracorporeal Shockwave Therapy (ESWT): This non-invasive procedure stimulates healing in the hip tissues using focused sound waves.
- Ultrasound-Guided Injections: Ensuring precision during corticosteroid or other therapeutic injections for maximum efficacy.
Surgical Intervention
Surgery is typically considered a last resort for trochanteric bursitis when other treatments fail. Options include:
- Bursa Removal: The inflamed bursa is removed to alleviate symptoms.
- Corrective Procedures: Addressing underlying structural issues contributing to the condition.
Prognosis and Long-Term Management
With appropriate treatment, most individuals with trochanteric bursitis experience significant improvement within weeks to months. To prevent recurrence:
- Maintain a Healthy Weight: Reducing excess body weight minimizes stress on the hips.
- Incorporate Regular Exercise: Focus on strengthening the hip abductors and improving core stability.
- Practice Proper Biomechanics: Correcting gait abnormalities and using proper posture can reduce stress on the bursa.
- Choose Supportive Footwear: Shoes with adequate cushioning and arch support can help.
When to Seek Professional Help
If hip pain persists or worsens despite conservative measures, it’s essential to consult a healthcare provider. Precision Pain Care and Rehabilitation specializes in diagnosing and treating musculoskeletal conditions like trochanteric bursitis using advanced interventional techniques.
Conclusion
Trochanteric bursitis is a manageable condition with the right combination of treatments and preventive strategies. By addressing the underlying causes and seeking timely medical intervention, individuals can restore mobility, reduce pain, and improve their quality of life.
For more information about managing hip pain or to schedule an appointment, visit Precision Pain Care and Rehabilitation.
Precision Pain Care and Rehabilitation has two convenient locations in Richmond Hill – Queens, and New Hyde Park – Long Island. Call the Queens office at (718) 215-1888 or (516) 419-4480 for the Long Island office to arrange an appointment with our Interventional Pain Management Specialists, Dr. Jeffrey Chacko or Dr. Sonny Ahluwalia.
Note: This article is for informational purposes only and should not be considered medical advice. Consult a healthcare professional for personalized recommendations.















