Osteoarthritis (OA) is a condition caused by the gradual wear and tear of joints over time. Multiple factors, including genetics, may increase your likelihood of developing this progressive disease.
Osteoarthritis affects over 32.5 million adults in the United States and is the most common form of arthritis, particularly in older adults. It’s also a leading cause of disability. If OA runs in your family, you may be at a higher risk of developing it.
In this guide, we will explore what OA is, how genetics contribute to the disease, and what other risk factors might influence its onset.
What is Osteoarthritis (OA)?
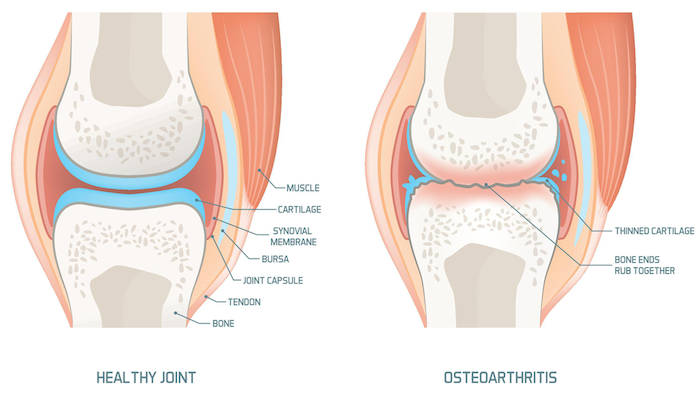
Cartilage is the cushioning tissue that sits between bones in your body’s joints. In osteoarthritis, this cartilage gradually breaks down over time. As the cushioning wears away, joints become more painful, and everyday activities may become more challenging and uncomfortable.
Symptoms of OA include:
- Joint pain that improves with rest
- Stiffness in the morning or after periods of inactivity
- Swelling in the affected joint after use
- Limited joint mobility and instability
- Pain during sleep (in later stages)
While there is no cure for OA, various treatments—such as lifestyle adjustments, medications, and surgery can help manage the condition.
Is Osteoarthritis Genetic?
There is a genetic component to OA. If you have a family history of the condition, your chances of developing OA are higher than those without that history. However, this doesn’t mean genetics are the sole cause. Other factors, including lifestyle, weight, and occupation, also play a significant role.
Researchers use a measure called "heritability" to understand how much genetic factors influence certain traits. Studies suggest that the heritability of OA varies by joint:
- Spine: 70%
- Hand: 65%
- Hip: 60%
- Knee: 40%
Which Genes Might Be Involved?
There are more than 100 gene variants associated with the development of OA. A 2015 review of studies identified several groups of genes related to key factors in OA development:
- Cartilage and Connective Tissue Structure
Variations in the genes COL2A1, COL9A3, and COL11A1 may affect the cartilage and connective tissues in your joints, making them wear out more quickly. These mutations are linked to faster degradation of cartilage, particularly in the knees and hips.
- Bone Density
Genes like the vitamin D receptor (VDR) and estrogen receptor alpha (ESR1) affect estrogen receptors and may increase your risk of OA. Variations in these genes could impact bone density and lead to OA, especially in the hands and knees.
- Chondrocyte Cell Signaling
Variations in the BMP5, FRZB, and IL-4Rα genes mainly affect women, raising their risk of OA in the hips, knees, and other joints.
- Inflammation
Genes such as IL-1, IL-10, TGFB1, IL-6, and TNFα influence inflammatory responses in the joint lining (synovium). Inflammation can lead to cartilage breakdown, particularly in the hands, knees, and hips.
Are There Other Causes of Osteoarthritis?
Yes, genetics is just one piece of the puzzle. Other factors can also contribute to OA:
- Joint Injuries or Abnormalities: Damage to joints or issues with joint structure can increase your risk.
- Occupation: Jobs that involve repetitive knee-bending, heavy lifting, or other strenuous physical activity may elevate your risk of developing OA over time.
Other Risk Factors for Osteoarthritis
In addition to genetics, other risk factors that can increase the likelihood of developing OA include:
- Age: The risk increases as you get older, with most cases occurring in people aged 50 and above.
- Gender: Women are more likely than men to develop OA.
- Weight: Obesity places extra strain on joints, particularly the knees and hips.
- Race: Some populations, such as certain Asian groups, may have a lower risk of OA.
- Health History: Previous injuries and overuse of joints can increase your chances of developing OA.
What is the Outlook for People with Osteoarthritis?
Although there is no cure for OA, it is a progressive disease that can worsen over time. However, proper treatment and lifestyle changes can help you manage the symptoms, maintain mobility, and improve your quality of life.
What Are Other Common Forms of Arthritis?
According to the Centers for Disease Control and Prevention (CDC), the most common types of arthritis apart from OA include gout, fibromyalgia, and rheumatoid arthritis.
Precision Pain Care and Rehabilitation has two convenient locations in Richmond Hill – Queens, and New Hyde Park – Long Island. Call the Queens office at (718) 215-1888 or (516) 419-4480 for the Long Island office to arrange an appointment with our Interventional Pain Management Specialists, Dr. Jeffrey Chacko or Dr. Sonny Ahluwalia.